Inflammatory Heart Disease
Inflammatory heart disease is increasingly recognised as one of the major causes of heart failure worldwide. Viral infections (influenza, cardiotropic viruses, HIV, COVID-19), chronic rheumatological conditions (lupus, rheumatoid arthritis, sarcoidosis), and previous cancer treatment are all recognised triggers of a persistent ‘low-flame’ inflammation of the heart muscle (myocarditis) and small vessels (vasculitis, microvascular disease). This is often accompanied by pericarditis, which is inflammation of the heart’s lining.
A Silent Disease
Unlike myocardial infarction, which manifests itself through excruciating chest pain, myocarditis is a silent (subclinical) disease process, which gives away very little symptoms. These are subtle and nonspecific:
- Effort intolerance
- Atypical chest pains more pronounced after a busy day or after exercise
- Struggling to regain fitness
- Resting tachycardia and/or excessive tachycardic response to exercise
After months of accumulating inflammatory injury, patients may eventually show overt cardiac symptoms, such as shortness of breath on minimal exertion or even signs of heart failure.
Early recognition is important because there is a good chance that early cardioprotective treatment could reduce the relentless course of inflammatory damage or even halt it.
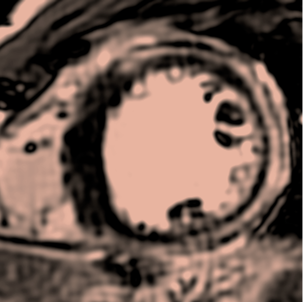
Cardiac MRI: The Gold Standard
Cardiac magnetic resonance is the diagnostic test of choice in inflammatory cardiomyopathies, because it is very sensitive to detect inflammation directly within the tissue of the heart. Dr Puntmann contributed numerous insights into the early detection of cardiac inflammation using cardiac magnetic resonance in the above-mentioned predisposing conditions.
The list of her publications can be found here.